
Today, no one is surprised by this methodtreatment, as a surgical intervention. But several centuries ago the operation was equated with death: most patients died of pain shock or sepsis. For a long time, the introduction of a person into a surgical sleep remained the most difficult task of medicine. With the study of chemistry, the process went faster. Better mixtures and preparations for anesthesia were created, which, in addition, are now carried out in various ways. One of them is endotracheal anesthesia. What it is? How is it used and in what cases is it necessary? These and many other questions will be answered in the article.
This type of anesthesia was first tested in XIV-XVcenturies, when a physician Paracelsus from Switzerland introduced a tube into the trachea of a man, than saved his life. Three centuries later, people were saved in such a way from lack of air. In 1942, an anesthesiologist from Canada for the first time used muscle relaxants - substances that reduce the tone of skeletal muscles until complete immobilization. Thanks to this discovery, anesthesia became safer and more perfect, allowing specialists to fully control the course of surgical sleep during the operation.
In the middle of the 20th century, endotracheal anesthesia becamerapidly develop, which contributed to the Soviet doctors. Today, this is the most common method of general anesthesia, used in the process of most operations.
In order to protect the body from the hugestress during surgery, use anesthesia. It can be local, regional or general. The latter is called anesthesia. It is characterized by a complete "shutdown" of the patient's consciousness with the onset of surgical sleep. In modern anesthesiology, intravenous, mask or combined anesthesia is used. The latter combines two methods: the substances enter both the blood and the respiratory tract. This form is called endotracheal anesthesia.

Experts rightfully consider it the safestand an effective method of anesthesia: it allows to fully control the patient's condition, achieve deep surgical sleep and relaxation of skeletal muscles, and also to avoid such unpleasant complications as aspiration and respiratory failure.
Endotracheal anesthesia protects the patient frompain shock and respiratory failure, which allows using it in the period of operations and resuscitation. Among the indications for combined anesthesia may be:
Endotracheal general anesthesia is more often usedfor long operations, the term of which is more than 30 minutes. It can be used at any age for different conditions of the patient, because it does not load the heart and is much less toxic to other methods of anesthesia.
Planned surgical treatment (for example,surgery to remove the tumor of the mediastinum) is accompanied by a thorough study of the patient's condition. The doctor has the necessary time to get acquainted with the patient's medical record, having time to calculate possible risks and to reveal contraindications to this or that method of anesthesia. Combined anesthesia is not recommended in the following conditions:
Especially dangerous is the use of endotracheal anesthesia in upper respiratory tract infections, because the risk of contracting the lungs is high.
So, endotracheal anesthesia.What is this for the doctor? An anesthesiologist performs three consecutive stages of action: introduction to surgical sleep, maintaining a stable state and awakening. The first stage consists in the implementation of a light initial anesthetic. The patient receives drugs intravenously or inhales a mixture of gases. When the muscles are completely relaxed, the anesthetist enters the intubation tube into the lumen of the trachea. It provides ventilation of the lungs with oxygen and inhalation with gaseous anesthetics.

After the surgeons have completed their work,there comes a crucial moment for the anesthesiologist - withdrawal of the patient from anesthesia. Dosage of drugs is gradually reduced. After restoration of independent breathing, extubation is carried out - removal of the intubation tube from the trachea. The patient is transported to the intensive care unit, observing the vital signs and the process of postoperative recovery.
Easy initial anesthesia is necessary forpainless and safe intubation, without the realization of which endotracheal anesthesia is impossible. To achieve this state, inhalations or intravenous pain medications are used. In the first case, the patient breathes through the mask with "Etran", "Forana", "Fluorotan" or other similar mixtures of anesthetics. Sometimes there is enough nitrous oxide with oxygen.
As medications administered intravenously,Barbiturates and neuroleptics (droperidol, fentanyl) are commonly used. They are used as a solution (not more than 1%). The dose of the drug is selected by the anesthesiologist individually for each patient.

After a slight anesthesia has affected,perform intubation of the trachea. For this, muscle relaxants are used to relax the muscles of the neck. The tube is injected with a laryngoscope, after which the patient is transferred to an artificial lung ventilation. The stage of deep anesthesia begins.
Droperidol is an antipsychotic commonly usedwith endotracheal anesthesia. By chemical structure, this substance is a tertiary amine. Has a sedative effect as early as 3 minutes after injection. It blocks dopamine receptors, which causes neurovegetative inhibition. In addition, it has antiemetic and hypothermic action. Breathing affects slightly.
It is prescribed for premedication, introductory anesthesia,myocardial infarction, shock state, severe angina pectoris, pulmonary edema and hypertensive crisis. It is recommended as a drug that eliminates nausea and vomiting. It has low toxicity, which allows it to be used in pediatric surgery and obstetrics.
There are several options for performingneyroleptanalgezii. Introduction anesthesia is usually carried out according to this scheme: droperidol, the instruction of which was discussed above, in the amount of 2-5 ml with 6-14 ml of fentanyl is administered intravenously to the patient. At the same time serves a mask with a mixture of nitrous oxide and oxygen in a ratio of 2: 1 or 3: 1. After depression of consciousness, muscle relaxants are administered and intubation is initiated.

Droperidol has a neuroleptic effect inwithin 4-5 hours, so it is administered at the beginning of the anesthesia. Calculate it based on body weight: 0.25-0.5 mg / kg. Repeated administration of the drug is necessary only for long operations.
Fentanyl in the amount of 0.1 mg is administered every 20 minutes and stops its delivery 30-40 minutes before the end of the surgery. The initial dose is 5-7 mcg / kg.
After the depression of consciousness, an artificialoxygen ventilation of the lungs using an anesthetic mask. Then the doctor performs intubation through the mouth (less often through the nose). The head is thrown back, the mouth is opened. A laryngoscope with a straight blade is inserted in the midline between the sky and the tongue, pressing the latter upwards. Moving the instrument further, lift the tip of the epiglottis. The glottis is shown in which the endotracheal tube is inserted. She should go into the trachea approximately 2-3 cm. After successful intubation, the tube is fixed and the patient is connected to the ventilator.
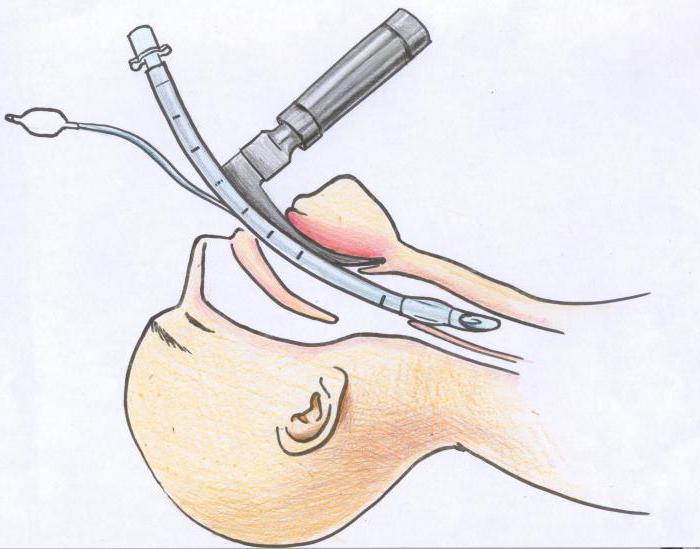
Less commonly used laryngoscope with a curved blade.It is inserted between the base of the epiglottis and the root of the tongue, squeezing the latter upwards from itself. If it is impossible to insert the tube through the mouth, use the lower nasal passage. For example, an operation is performed to remove a cyst of the oral cavity.
After intubation and connecting the patient to the deviceIVL comes the main period. Surgeons are actively working, the anesthesiologist is closely monitoring livelihoods. Every 15 minutes check the heart rate, blood pressure, with the help of monitors monitor the patient's heart activity.
General anesthesia is maintained byadditional doses of neuroleptics, muscle relaxants or inhalations with mixtures of anesthetics. The operation under combined anesthesia allows the anesthesiologist to adapt to the needs of the body in anesthesia, providing an optimal level of safety.
After the end of surgical procedurescomes the last stage - out of narcotic sleep. Before the onset of this point smoothly reduce the dosage of drugs. Atropine and prozerin are administered at 5-minute intervals to restore breathing. Making sure that the patient is able to breathe on their own, they carry out extubation. To do this, clear the area of the tracheobronchial tree. After removal of the tube, a similar procedure is performed with the oral cavity.

After leaving the operating room, the patient is placed inintensive care unit, where it is carefully monitored for its condition. After general anesthesia, unpleasant sensations develop, less often complications. Usually, postoperative patients complain of:
These symptoms usually disappear within the first 2-48 hours after surgery. To eliminate the pain prescribed analgesics.

So let's summarize.Endotracheal anesthesia - what is it? This is a method of introducing a person into a surgical sleep, allowing to perform complex operations, controlling the activity of the respiratory system. Combined anesthesia is less toxic, and the depth of anesthesia is easy to control during the entire period of intervention. By endotracheal anesthesia primarily imply intubation followed by connecting the patient to the ventilator. It uses both inhaled and drug anesthetics, which are usually combined.


























