
Sexually transmitted diseases are widelycommon among both men and women. They are not only accompanied by unpleasant sensations in the genital area, but also are hazardous to health. Long-term chronic infections can result in infertility. One of the venereal pathologies is chlamydia. This disease can occur in different ways, depending on the serotype of the pathogen. In some cases, the manifestation of infection is venereal lymphogranuloma. This pathology is found in tropical countries, parts of America and Asia. However, episodic outbreaks of infection can be observed everywhere.
The disease refers to sexually transmitted infections.It has several names. Among them: climatic bubo, inguinal lymphogranulomatosis, Duran-Nicola-Favre disease. Previously, this pathology was called "the fourth venereal infection", since it became known about it after syphilis, soft chancre and gonorrhea. In most cases, the disease is sexually transmitted. Venereal lymphogranuloma occurs in both sexes. However, more often it is observed in men.

Данная патология относится к инфекциям, sexually transmitted. The causative agent of the disease is chlamydia trachomatis. This microorganism is represented by various serological species. The cause of venereal lymphogranuloma are types L1,2 and 3. Symptoms of the disease are different from urogenital chlamydia caused by the same pathogen. This is due to the fact that these serotypes have tropism for lymphoid tissue. Since pathology is a venereal disease, the main cause of infection is sexual contact with an infected partner. The pathogen enters the body through damaged skin and mucous membranes. The appearance of the first symptoms can be observed both on the genitals and in the oral cavity and rectum. The spread of infection is also possible with the transfusion of infected blood, cosmetic procedures.
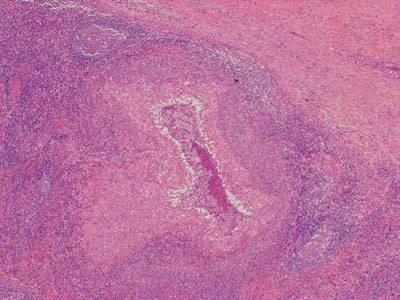
Venereal lymphogranuloma does not develop immediately.Like many infectious pathologies, the disease has an incubation period. It can last from several days to 2 months. After the pathogen enters the body through the damaged tissue, the infection begins to spread through the lymphatic vessels. Chlamydia multiply rapidly and cause necrosis and tissue inflammation. Since they have an affinity for the lymph nodes, all these changes occur there. Lymphadenitis is often symmetrical. Later, the inflammatory process goes to the skin. With a long-term current infection and no treatment, the pathogen spreads from the lymphatic vessels into the bloodstream. In this case, chlamydia persist throughout the body. This is a very dangerous symptom, as it leads to serious complications.

The first signs of the disease appear inincubation period. They are characterized by fever, weakness, myalgia. Later, local symptoms of infection join. At the same time on the skin and mucous membranes there are rashes in the form of pustules, papules and vesicles. Venereal chlamydial lymphogranuloma in men usually begins with the head of the penis or coronary sulcus. Sometimes the place of infection is the foreskin. In women, rashes can appear on the skin of the labia or vagina. In non-traditional sexual intercourse, the place of implantation becomes: the mucous membrane of the cheeks, the tonsils, the rectal area. After a few days, the rashes disappear on their own, leaving no traces or discomfort. For this reason, patients often do not notice that they have been infected. After 2-6 weeks, lymph nodes are affected. They become painful and increased in size. Palpation of the lymph nodes are soldered to the surrounding tissues. In most cases, the lesion begins on one side and quickly spreads to the opposite half. The inflammatory process may include the inguinal, iliac, femoral lymph nodes (sometimes - the submandibular, cervical groups). This process is accompanied by symptoms of intoxication. Later, chlamydial venereal granuloma enters the terminal stage. The pathogen spreads throughout the body, affecting tissue. There is a formation of fistulas, inflammation of the fiber of the rectum, stagnation of lymph. At the same time complications often develop.

Диагностика хламидийной лимфогранулемы based on history and clinical picture. It is necessary to find out: did the patient have unprotected sex and rash on the genitals. Symptoms can be confused with other pathologies, such as lymphogranulomatosis, syphilis and genital herpes. Therefore, in addition to assessing the clinical situation, laboratory diagnosis is necessary. Materials for the study are blood, discharge from pustules and vesicles, tissue of the lymph node. Since cross-reaction with other types of chlamydia is possible, serological diagnostic methods are necessary. In the laboratory, the pathogen is grown on chicken embryos (culture analysis).
It must be remembered that the disease is highcontagious. Therefore, the treatment of venereal lymphogranuloma should be carried out by both partners simultaneously. At this time, sex should be excluded. Etiological treatment is considered antibiotic therapy. Apply drugs "Hemomitsin", "Erythromycin". Dieting is also necessary (exclude sweet, bitter and salty foods). With the development of complications, surgical manipulations are performed: opening and drainage of the lymphatic vessels. In case of erosive surfaces on the skin, local treatment (antiseptic baths) and frequent change of linen are necessary.

To avoid infection, carry out the primary prevention of infection. This includes the following measures:
To avoid complications, conduct secondary prevention. It consists in the strict fulfillment of the doctor's prescriptions, and the simultaneous treatment of partners.
Venereal lymphogranuloma dangerous developmentsevere complications. Usually they develop in the terminal stage of the disease, with no treatment. With destruction of the lymph nodes, complications such as paraproctitis, elephantiasis, fistulas and adhesions are observed. This leads to intestinal obstruction. If the pathogen enters the bloodstream, inflammation of organs and systems is possible. The most dangerous complication is the penetration of chlamydia in the brain tissue.


























